Levator ani
This article may require cleanup to meet Wikipedia's quality standards. The specific problem is: Content under Pubococcygeus and Puborectalis sections should be integrated with the rest of the article. (July 2020) |
| Levator ani | |
|---|---|
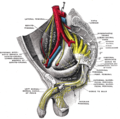
 Left levator ani seen from within. | |
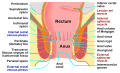
 Coronal section through the male anal canal. B. Cavity of urinary bladder V.D. Vas deferens. S.V. Seminal vesicle. R. Second part of rectum. A.C. Anal canal. L.A. Levator ani. I.S. Internal anal sphincter. E.S External anal sphincter. | |
| Details | |
| Origin | Inner surface of the side of the lesser pelvis |
| Insertion | Inner surface of coccyx, levator ani of opposite side, and into structures that penetrate it. |
| Artery | Inferior gluteal artery |
| Nerve | Pubococcygeus and iliococcygeus: |
| Actions | Supports the viscera in pelvic cavity |
| Identifiers | |
| Latin | musculus levator ani |
| TA98 | A04.5.04.002 |
| TA2 | 2403 |
| FMA | 19087 |
| Anatomical terms of muscle | |

The levator ani is a broad, thin muscle group, situated on either side of the pelvis. It is formed from three muscle components: the pubococcygeus, the iliococcygeus, and the puborectalis.[3]
It is attached to the inner surface of each side of the lesser pelvis, and these unite to form the greater part of the pelvic floor. The coccygeus muscle completes the pelvic floor, which is also called the pelvic diaphragm.
It supports the viscera in the pelvic cavity, and surrounds the various structures that pass through it.
The levator ani is the main pelvic floor muscle and contracts rhythmically during female orgasm, and painfully during vaginismus.[4]
Structure
[edit]The levator ani is made up of 3 parts:
- Iliococcygeus muscle
- Pubococcygeus muscle
- Puborectalis muscle
The iliococcygeus arises from the inner side of the ischium (the lower and back part of the hip bone) and from the posterior part of the tendinous arch of the obturator fascia, and is attached to the coccyx and anococcygeal body; it is usually thin, and may be absent, or be largely replaced by fibrous tissue. An accessory slip at its posterior part is sometimes named the iliosacralis.
The pubococcygeus muscle has medial fibres forming the pubovaginalis in the female, and the puboprostaticus in the male.
Origin and insertion
[edit]The levator ani arises, in front, from the posterior surface of the superior pubic ramus lateral to the symphysis; behind, from the inner surface of the spine of the ischium; and between these two points, from the obturator fascia.
Posteriorly, this fascial origin corresponds, more or less closely, with the tendinous arch of the pelvic fascia, but in front, the muscle arises from the fascia at a varying distance above the arch, in some cases reaching nearly as high as the canal for the obturator vessels and nerve.
The fibers pass downward and backward to the middle line of the floor of the pelvis; the most posterior are inserted into the side of the last two segments of the coccyx; those placed more anteriorly unite with the muscle of the opposite side, in a median fibrous ridge called the anococcygeal body or raphe, which extends between the coccyx and the margin of the anus.
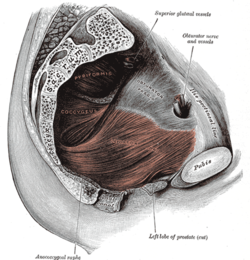
The middle fibers are inserted into the side of the rectum, blending with the fibers of the sphincter muscles; lastly in the male, the anterior fibers descend upon the side of the prostate to unite beneath it with the muscle of the opposite side, joining with the fibers of the external anal sphincter and transverse perineal muscles, at the central tendinous point of the perineum.
The anterior portion is occasionally separated from the rest of the muscle by connective tissue.
From this circumstance, as well as from its peculiar relation with the prostate, which it supports as in a sling, it has been described as a distinct muscle, under the name of levator prostatæ.
In the female, the anterior fibers of the levator ani descend upon the side of the vagina.
Innervation
[edit]The levator ani muscles are mostly innervated by the pudendal nerve, perineal nerve and acting together.[5]
Variation
[edit]In addition, sacral spinal nerves (S3, S4) innervate the muscles directly as well (in ~70%[5] of people). Sometimes (in ~40%[5] of people) the inferior rectal nerve innervates the levator ani muscles independently of the pudendal nerve.
Pubococcygeus muscle
[edit]| Pubococcygeus muscle | |
|---|---|
| Details | |
| Origin | back of the pubis and from the anterior part of the obturator fascia |
| Insertion | coccyx and sacrum |
| Nerve | S3, S4 |
| Actions | controls urine flow and contracts during orgasm |
| Identifiers | |
| Latin | musculus pubococcygeus |
| TA98 | A04.5.04.002 |
| TA2 | 2403 |
| FMA | 19087 |
| Anatomical terms of muscle | |
The pubococcygeus muscle or PC muscle is a hammock-like muscle, found in both sexes, that stretches from the pubic bone to the coccyx (tail bone) forming the floor of the pelvic cavity and supporting the pelvic organs.
Structure
[edit]The pubococcygeus arises from the back of the pubis and from the anterior part of the obturator fascia, and is directed backward almost horizontally along the side of the anal canal toward the coccyx and sacrum, to which it finds attachment.
Between the termination of the vertebral column and the anus, the two pubococcygeus muscles come together and form a thick, fibromuscular layer lying on the raphe (ridge) or (anococcygeal body) formed by the iliococcygei.
The greater part of this muscle is inserted into the coccyx and into the last one or two pieces of the sacrum.
Variation
[edit]This insertion into the vertebral column is, however, not accepted by all observers.
Function
[edit]The pubococcygeus muscle controls urine flow and contracts during orgasm as well as assisting in male ejaculation.[6] It also aids in childbirth as well as core stability.[7]
A strong pubococcygeus muscle has also been linked to a reduction in urinary incontinence and proper positioning of the baby's head during childbirth.
Kegel exercises
[edit]The Kegel exercises are a series of voluntary contractions of all the perineal muscles. Such movement is done in an effort to strengthen all the striated muscles in the perineum's area. They are often referred to simply as "kegels", named after their founder, Dr. Arnold Kegel.[8] These exercises also serve to contract, among others, the ischiocavernosus, bulbospongiosus, and cremaster muscle in men, as voluntary contraction of the pubococcygeus muscle also engages the cremasteric reflex, which lifts the testicles up, although this does not occur in all men. Kegel exercises have been prescribed to ameliorate erectile dysfunction due to venous leakage and to help men control premature ejaculation[9] and to treat urinary incontinence in both sexes.[10][needs update][11]
Puborectalis muscle
[edit]| Puborectalis muscle | |
|---|---|
 The posterior aspect of the rectum exposed by removing the lower part of the sacrum and the coccyx. (Puborectalis not labeled but levator ani labeled at bottom right and external anal sphincter labeled at bottom center.) | |
| Details | |
| Origin | lower part of the pubic symphysis, superior fascia of the urogenital diaphragm |
| Nerve | S3, S4. levator ani nerve[12] |
| Actions | inhibit defecation |
| Identifiers | |
| Latin | musculus puborectalis |
| TA98 | A04.5.04.002 |
| TA2 | 2403 |
| FMA | 19087 |
| Anatomical terms of muscle | |
The fibers that form a sling looping around the rectum are named puborectalis (puboanalis). They arise from the lower part of the pubic symphysis, and from the superior fascia of the urogenital diaphragm. The origin of the puborectalis fibers is at the posterior surface of the pubis while their insertion is at the midline sling posterior to the rectum. The muscle band is innervated by perineal branches of the S3 and S4 nerve roots.
They meet with the corresponding fibers of the opposite side around the lower part of the rectum, and form for it a strong sling. Relaxation increases the angle between rectum and anus, allowing defecation in conjunction with relaxation of the internal and external anal sphincters. Levator ani relaxation and rectal emptying is facilitated by anorectal straightening during squatting.[13]
Function
[edit]The levator ani muscles are responsible for "wagging" the tail in tailed quadrupeds. These muscles are not as strong in the human, as tail-wagging is more demanding than the support function that the muscles serve in humans.[14]
Clinical significance
[edit]Levator ani syndrome
[edit]Levator ani syndrome is episodic rectal pain caused by spasm of the levator ani muscle.[15][16][17]
Levator ani avulsion
[edit]This section is empty. You can help by adding to it. Find sources: "Levator ani avulsion" – news · newspapers · books · scholar · JSTOR (January 2024) |
Additional images
[edit]-
Right hip bone. Internal surface.
-
Coronal section of pelvis, showing arrangement of fasciæ. Viewed from behind.
-
Muscles of male perineum.
-
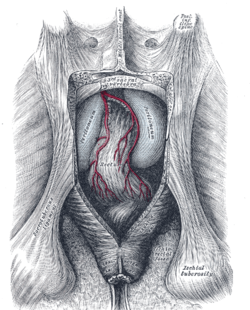
The arteries of the pelvis.
-
Sacral plexus of the right side.
-
Iliac colon, sigmoid or pelvic colon, and rectum seen from the front, after removal of pubic bones and bladder.
-
The posterior aspect of the rectum exposed by removing the lower part of the sacrum and the coccyx.
-
Male pelvic organs seen from right side.
-
Anatomy of the human anus.
See also
[edit]References
[edit]![]() This article incorporates text in the public domain from page 422 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 422 of the 20th edition of Gray's Anatomy (1918)
- ^ Essential Clinical Anatomy. K.L. Moore & A.M. Agur. Lippincott, 2nd ed. 2002. Page 217
- ^ Wallner C, Maas C, Dabhoiwala N, Lamers W, Deruiter M (2006). "Evidence for the innervation of the puborectalis muscle by the levator ani nerve". Neurogastroenterol Motil. 18 (12): 1121–1122. doi:10.1111/j.1365-2982.2006.00846.x. PMID 17109696. S2CID 29088779.
- ^ Drake, Richard; Vogl, A. Wayne; Mitchell, Adam (2015). Gray's Anatomy for Students (Third ed.). Elsevier.
- ^ Christopher R. Chapple (2006). Multidisciplinary Management of Female Pelvic Floor Disorders. Churchill Livingstone. pp. 4–. ISBN 978-0-443-07272-7.
- ^ a b c Grigorescu BA, Lazarou G, Olson TR, et al. (2008). "Innervation of the levator ani muscles: description of the nerve branches to the pubococcygeus, iliococcygeus, and puborectalis muscles". Int Urogynecol J Pelvic Floor Dysfunct. 19 (1): 107–116. doi:10.1007/s00192-007-0395-8. PMID 17565421. S2CID 21118078.
- ^ Marieb, Elaine (2013). Anatomy & physiology : books a la carte edition. Benjamin-Cummings. p. 895. ISBN 9780321887603.
- ^ "Core stabilization, Core Coordination, article by Aline Newton, M.A., certified Advanced Rolfer, the biomechanics of core stabilization, with core as a center of movement instead of a center of holding". Alinenewton.com. Retrieved 2012-02-20.
- ^ Kegel exercises Gannet Health Services. Cornwell University website
- ^ How To do Kegel Exercises (for men) Silverberg, Corey. About.com
- ^ Dumoulin, Chantale; Hay-Smith, E. Jean C.; Mac Habée-Séguin, Gabrielle (2014-05-14). "Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women". The Cochrane Database of Systematic Reviews (5): CD005654. doi:10.1002/14651858.CD005654.pub3. hdl:1866/33736. ISSN 1469-493X. PMID 24823491.
- ^ Anderson, Coral A.; Omar, Muhammad Imran; Campbell, Susan E.; Hunter, Kathleen F.; Cody, June D.; Glazener, Cathryn M. A. (2015-01-20). "Conservative management for postprostatectomy urinary incontinence". The Cochrane Database of Systematic Reviews. 1 (1): CD001843. doi:10.1002/14651858.CD001843.pub5. hdl:2164/6141. ISSN 1469-493X. PMC 7025637. PMID 25602133.
- ^ Wallner C, Maas C, Dabhoiwala N, Lamers W, Deruiter M (2006). "Evidence for the innervation of the puborectalis muscle by the levator ani nerve". Neurogastroenterol Motil. 18 (12): 1121–2. doi:10.1111/j.1365-2982.2006.00846.x. PMID 17109696. S2CID 29088779.
- ^ Modi, Rohan M.; Hinton, Alice; Pinkhas, Daniel; Groce, Royce; Meyer, Marty M.; Balasubramanian, Gokulakrishnan; Levine, Edward; Stanich, Peter P. (March 2019). "Implementation of a Defecation Posture Modification Device". Journal of Clinical Gastroenterology. 53 (3): 216–219. doi:10.1097/MCG.0000000000001143. ISSN 0192-0790. PMC 6382038. PMID 30346317.
- ^ Sloan, Ethel (2001, p. 53). Biology of Women, Wisconsin: CENGAGE Delmar Learning. ISBN 0-7668-1142-5 (excerpt available here Archived 2006-05-21 at the Wayback Machine)
- ^ Levator Syndrome, by Parswa Ansari, MD 7/2014, Merck Manuals
- ^ Giulio Aniello Santoro; Andrzej Paweł Wieczorek; Clive I. Bartram (27 October 2010). Pelvic Floor Disorders: Imaging and Multidisciplinary Approach to Management. Springer. p. 601. ISBN 978-88-470-1542-5.
- ^ Bharucha AE, Trabuco E (September 2008). "Functional and chronic anorectal and pelvic pain disorders". Gastroenterology Clinics of North America. 37 (3): 685–96, ix. doi:10.1016/j.gtc.2008.06.002. PMC 2676775. PMID 18794003.
- ^ Rusavy, Z; Paymova, L; Kozerovsky, M; Veverkova, A; Kalis, V; Kamel, RA; Ismail, KM (2021). "Levator ani avulsion: a Systematic evidence review (LASER)". BJOG: An International Journal of Obstetrics & Gynaecology. 129 (4). Wiley: 517–528. doi:10.1111/1471-0528.16837. ISSN 1470-0328. PMID 34245656.
External links
[edit]- Anatomy figure: 41:05-00 at Human Anatomy Online, SUNY Downstate Medical Center—"Muscles of the female superficial perineal pouch."
- Anatomy figure: 42:04-00 at Human Anatomy Online, SUNY Downstate Medical Center—"Muscles of the male superficial perineal pouch."
- Anatomy photo:43:16-0102 at the SUNY Downstate Medical Center—"Muscles of the Pelvic Diaphragm"
- Anatomy image:9072 at the SUNY Downstate Medical Center
- Anatomy image:9089 at the SUNY Downstate Medical Center
- Anatomy image:9871 at the SUNY Downstate Medical Center
- Cross section image: pelvis/pelvis-e12-15—Plastination Laboratory at the Medical University of Vienna
- perineum at The Anatomy Lesson by Wesley Norman (Georgetown University) (analtriangle3) * pelvis at The Anatomy Lesson by Wesley Norman (Georgetown University) (femalepelvicdiaphragm, malepelvicdiaphragm)
- Merck Manual article on levator ani syndrome