Nasal chondrocytes
Nasal chondrocytes (NC) are present in the hyaline cartilage of the nasal septum and in fact are the only cell type within the tissue. Similar to chondrocytes present in articular cartilage, NC express extracellular matrix proteins such as glycosaminoglycans and collagen.[1]
In their natural environment
[edit]At birth the nasal septum, except for the vomer ‘’anlage” is completely cartilaginous. In the second half of the first year of life, the septum progressively ossifies in posterior-anterior direction by a process of endochondral ossification.[2] The remaining cartilaginous part (characterized as hyaline cartilage) of the human nasal septum has a specific three-dimensional organization with regards to local differences in cell size and the amounts of extracellular matrix. In the outer region of the cartilage, NC are numerous, small, flat and oriented parallel to the surface. In the intermediate and central regions, NC are spheroid in shape, less dense, and are aligned perpendicular to the cartilage surface.[3] The cartilage matrix is mainly composed of type II collagen (90-95%), although small amounts of type IX and XI collagen are also found.[4] Nasal cartilage is tightly connected to perichondrium, consisting of several layers of connective tissue fibers (mainly based on type I collagen) running parallel to the cartilage.[5]
Tissue engineering applications
[edit]Articular chondrocytes have typically been the cell type used for cartilage tissue engineering strategies for articular cartilage repair. Since NC can also express hyaline cartilage specific extracellular matrix proteins such as glycosaminoglycans and collagen, NC have recently also been used for the in vitro engineering of cartilage tissues.
Cell isolation
[edit]Harvesting of nasal cartilage is minimally invasive, can be performed in an outpatient procedure under local anesthesia and is associated with minimal morbidity.[6] NC can be isolated from nasal septal cartilage biopsies by enzymatic digestion using collagenase type I, II or IV (at different combination and concentration – varying from 0.15% to 0.6% –) alone or after an initial short pre-incubation phase with pronase (0.2% - 1%).[7][8][9][10][11][12] Cell yield after enzymatic digestion of the nasal cartilage was estimated to be 2,100 - 3,700 cells/mg of tissue.[7][12] Alternatively, NC can be isolated by outgrowth culture of nasal cartilage fragments.[8]
Cell expansion
[edit]After isolation from septal cartilage biopsies, NC can be extensively expanded in numbers by conventional in vitro cell culture methods (monolayer culture in flasks or Petri dishes). The proliferation rate of NC was reported to be increased in the presence of specific growth factors such as TGF-beta and FGF-2[12][13] or culture supplements like Insulin-Transferrin-Selenium.[7] NC cultured in medium containing autologous serum exhibit similar proliferation rates to NC cultured with medium supplemented with fetal bovine serum.[13] Although articular chondrocytes derived from older individuals have been shown to have a lower proliferation capacity than from younger donors, NC have been shown to have significantly less age-dependence.[13][14]
Differentiation
[edit]Similar to other chondrocytes from hyaline cartilage tissues in other locations in the human body, NC undergo a process of cell de-differentiation during monolayer culture. NC de-differentiation can be characterized by a gradual acquisition of a fibroblastic morphology, the expression of proteins associated with an undifferentiated mesenchymal cell phenotype (e.g., type I collagen and versican), and decreased expression of hyaline cartilage proteins (e.g., type II collagen and aggrecan).[9] However, NC can re-differentiate when transferred back into a more physiological three-dimensional environment. Abundant production of cartilage specific matrix has been reported by expanded NC when induced to re-differentiate in micromass pellets,[11][12][14][15] alginate beads,[16][17][18][19][20] hydrogels,[7][21] or into porous scaffolds based on polyglycolic acid,[9][19][22] polyethylene glycol terephthalate/polybuthylene terephalate,[23] collagen,[24] or hyaluronic acid.[1][14][25] Supplementation with specific growth factors (e.g., TGF-beta, IGF-1, and GDF-5) during re-differentiation has been shown to enhance the accumulation of glycosaminoglycans (GAG) and type II collagen as well as the biomechanical properties of the generated constructs.[20][26]
Autologous serum has also been used during NC re-differentiation in place of fetal bovine serum with similar efficacy.[14][26][27] Studies that directly compared the re-differentiation of articular chondrocytes to NC have shown that the cartilage forming capacity of NC was higher and more reproducible than that of articular chondrocytes[24][25][28] with lower donor-related dependency.[13][14] Additionally NC have been recently shown to exhibit features of self-renewal capability, being able to form cartilage tissue following serial cloning possibly due to their neuro-ectodermal origin.[29]
Animal studies
[edit]Pre-clinical investigations have been undertaken using various animal models to provide proof-of-principle of the clinical potential of NC-based tissue engineered constructs for cartilage reconstruction. The maturation of human NC engineered grafts has often been assessed in the subcutaneous pocket of nude mice, i.e., an environment highly vascularized and permissive to, but not inductive of, chondrogenesis.[30][31] The extent of cartilage matrix production and the mechanical properties of NC-based constructs have been reported to increase in such ectopic in vivo models.[21][13][18][22][32][33][34] An ectopic mouse model was also used in order to test the effects of different production methods for generating large clinically relevant-sized NC-based tissue grafts.[26]
Although these models can yield insightful results, nude mice are not capable of eliciting a significant immune response, and therefore these studies cannot predict the prognosis of implanted engineered septal cartilage in an immunocompetent host. As an alternative, an orthotopic rat model has been established to study nasal septum repair. In this model, septal cartilage was first perforated to create a defect, and subsequently, an engineered cartilage graft implanted into the defect during the same surgical procedure[35]
Using an orthotopic large animal model to study repair of articular cartilage defects, engineered NC-based cartilage grafts were implanted into the condyle of goats. In this study, it was determined that NC directly contributed to the repair of the articular cartilage defects and resulted in a superior outcome as compared to engineered articular chondrocyte-based grafts.[36]
Clinical applications
[edit]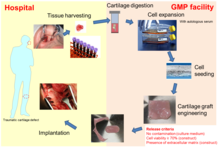
Engineered cartilage tissue, based on autologous NC, has recently been used by plastic surgeons for the reconstruction of nasal cartilage defects. Tissue engineered cartilage grafts based on NC as autologous grafts for the reconstruction of the alar lobule of the nose after skin tumor resection in a first-in-man clinical trial (ClinicalTrials.gov, number NCT01242618)[29] (see figure on the right). Their results demonstrated that the engineered grafts could lead to complete structural, functional and aesthetic satisfaction. Moreover, since harvesting of the nasal cartilage biopsy was minimally invasive, it could be performed in an outpatient procedure under local anesthesia, and was therefore associated with minimal morbidity.[6]
Several studies have demonstrated that NC are compatible with the environmental features typical of the injured knee (e.g., in terms of response to inflammatory molecules, mechanical loading and genetic molecular signature).[24][25][30] Thus nasal chondrocytes have been proposed as an alternative cell source for the repair of articular cartilage defects. A phase I clinical trial (ClinicalTrials.gov, number NCT 01605201) was conducted to test the safety and feasibility of implanting a tissue engineered cartilage graft based on autologous nasal chondrocytes for the regeneration of knee cartilage defects. The clinical observations of the first 10 patients of this study indicated not only safety and feasibility of the procedure, but together with Magnetic Resonance Imaging (MRI) and delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC) data, also showed promising results for efficacy of the treatment as indicated by significant improvement in clinical scores and regeneration of hyaline repair tissue after 24 months.[37] Based on this study, a multi-center phase II clinical trial was initiated and is currently ongoing to assess the efficacy of the NC-based cartilage grafts for the repair of traumatic knee cartilage defects (BIO-CHIP; funded by the European Union through the Horizon 2020 program, grant number 681103).
References
[edit]- ^ a b Candrian C, Vonwil D, Barbero A, Bonacina E, Miot S, Farhadi J, et al. (January 2008). "Engineered cartilage generated by nasal chondrocytes is responsive to physical forces resembling joint loading". Arthritis and Rheumatism. 58 (1): 197–208. doi:10.1002/art.23155. PMID 18163475.
- ^ Pelttari K, Mumme M, Barbero A, Martin I (October 2017). "Nasal chondrocytes as a neural crest-derived cell source for regenerative medicine". Current Opinion in Biotechnology. 47: 1–6. doi:10.1016/j.copbio.2017.05.007. PMID 28551498.
- ^ Schultz-Coulon HJ, Eckermeier L (January 1976). "Zum Postnatalen Wachstum Der Nasenscheidewand" [Postnatal growth of nasal septum]. Acta Oto-Laryngologica (in German). 82 (1–2): 131–142. doi:10.3109/00016487609120872. PMID 948977.
- ^ Popko M, Bleys RL, De Groot JW, Huizing EH (June 2007). "Histological structure of the nasal cartilages and their perichondrial envelope. I. The septal and lobular cartilage". Rhinology. 45 (2): 148–152. PMID 17708463.
- ^ Holden PK, Liaw LH, Wong BJ (July 2008). "Human nasal cartilage ultrastructure: characteristics and comparison using scanning electron microscopy". The Laryngoscope. 118 (7): 1153–1156. doi:10.1097/MLG.0b013e31816ed5ad. PMC 4151991. PMID 18438266.
- ^ a b Aksoy F, Yildirim YS, Demirhan H, Özturan O, Solakoglu S (January 2012). "Structural characteristics of septal cartilage and mucoperichondrium". The Journal of Laryngology and Otology. 126 (1): 38–42. doi:10.1017/S0022215111002404. PMID 21888752.
- ^ a b c d Siegel NS, Gliklich RE, Taghizadeh F, Chang Y (February 2000). "Outcomes of septoplasty". Otolaryngology–Head and Neck Surgery. 122 (2): 228–232. doi:10.1016/S0194-5998(00)70244-0. PMID 10652395. S2CID 43019892.
- ^ a b Chua KH, Aminuddin BS, Fuzina NH, Ruszymah BH (June 2005). "Insulin-transferrin-selenium prevent human chondrocyte dedifferentiation and promote the formation of high quality tissue engineered human hyaline cartilage". European Cells & Materials. 9: 58–67, discussion 67. doi:10.22203/ecm.v009a08. PMID 15962238.
- ^ a b c Elsaesser AF, Schwarz S, Joos H, Koerber L, Brenner RE, Rotter N (2016). "Characterization of a migrative subpopulation of adult human nasoseptal chondrocytes with progenitor cell features and their potential for in vivo cartilage regeneration strategies". Cell & Bioscience. 6: 11. doi:10.1186/s13578-016-0078-6. PMC 4752797. PMID 26877866.
- ^ Homicz MR, Schumacher BL, Sah RL, Watson D (November 2002). "Effects of serial expansion of septal chondrocytes on tissue-engineered neocartilage composition". Otolaryngology–Head and Neck Surgery. 127 (5): 398–408. doi:10.1067/mhn.2002.129730. PMID 12447233. S2CID 24779895.
- ^ a b Liese J, Marzahn U, El Sayed K, Pruss A, Haisch A, Stoelzel K (June 2013). "Cartilage tissue engineering of nasal septal chondrocyte-macroaggregates in human demineralized bone matrix". Cell and Tissue Banking. 14 (2): 255–266. doi:10.1007/s10561-012-9322-4. PMID 22714645. S2CID 254381658.
- ^ a b c d Shafiee A, Kabiri M, Ahmadbeigi N, Yazdani SO, Mojtahed M, Amanpour S, Soleimani M (December 2011). "Nasal septum-derived multipotent progenitors: a potent source for stem cell-based regenerative medicine". Stem Cells and Development. 20 (12): 2077–2091. doi:10.1089/scd.2010.0420. PMID 21401444.
- ^ a b c d e Wolf F, Haug M, Farhadi J, Candrian C, Martin I, Barbero A (February 2008). "A low percentage of autologous serum can replace bovine serum to engineer human nasal cartilage". European Cells & Materials. 15: 1–10. doi:10.22203/ecm.v015a01. PMID 18247273.
- ^ a b c d e Vinatier C, Magne D, Moreau A, Gauthier O, Malard O, Vignes-Colombeix C, et al. (January 2007). "Engineering cartilage with human nasal chondrocytes and a silanized hydroxypropyl methylcellulose hydrogel". Journal of Biomedical Materials Research. Part A. 80 (1): 66–74. doi:10.1002/jbm.a.30867. PMID 16958048.
- ^ Bujía J, Pitzke P, Kastenbauer E, Wilmes E, Hammer C (1996). "Effect of growth factors on matrix synthesis by human nasal chondrocytes cultured in monolayer and in agar". European Archives of Oto-Rhino-Laryngology. 253 (6): 336–340. doi:10.1007/BF00178288. PMID 8858257. S2CID 12243849.
- ^ Peñuela L, Wolf F, Raiteri R, Wendt D, Martin I, Barbero A (June 2014). "Atomic force microscopy to investigate spatial patterns of response to interleukin-1beta in engineered cartilage tissue elasticity". Journal of Biomechanics. 47 (9): 2157–2164. doi:10.1016/j.jbiomech.2013.10.056. PMID 24290139.
- ^ Alexander TH, Sage AB, Schumacher BL, Sah RL, Watson D (September 2006). "Human serum for tissue engineering of human nasal septal cartilage". Otolaryngology–Head and Neck Surgery. 135 (3): 397–403. doi:10.1016/j.otohns.2006.05.029. PMID 16949971. S2CID 383736.
- ^ a b Rotter N, Bonassar LJ, Tobias G, Lebl M, Roy AK, Vacanti CA (August 2002). "Age dependence of biochemical and biomechanical properties of tissue-engineered human septal cartilage". Biomaterials. 23 (15): 3087–3094. doi:10.1016/s0142-9612(02)00031-5. PMID 12102179.
- ^ a b Chang AA, Reuther MS, Briggs KK, Schumacher BL, Williams GM, Corr M, et al. (January 2012). "In vivo implantation of tissue-engineered human nasal septal neocartilage constructs: a pilot study". Otolaryngology–Head and Neck Surgery. 146 (1): 46–52. doi:10.1177/0194599811425141. PMC 4352411. PMID 22031592.
- ^ a b Homicz MR, Chia SH, Schumacher BL, Masuda K, Thonar EJ, Sah RL, Watson D (January 2003). "Human septal chondrocyte redifferentiation in alginate, polyglycolic acid scaffold, and monolayer culture". The Laryngoscope. 113 (1): 25–32. doi:10.1097/00005537-200301000-00005. PMID 12514377. S2CID 24972306.
- ^ a b Tay AG, Farhadi J, Suetterlin R, Pierer G, Heberer M, Martin I (2004). "Cell yield, proliferation, and postexpansion differentiation capacity of human ear, nasal, and rib chondrocytes". Tissue Engineering. 10 (5–6): 762–770. doi:10.1089/1076327041348572. PMID 15265293.
- ^ a b van Osch GJ, Marijnissen WJ, van der Veen SW, Verwoerd-Verhoef HL (2001). "The potency of culture-expanded nasal septum chondrocytes for tissue engineering of cartilage". American Journal of Rhinology. 15 (3): 187–192. doi:10.2500/105065801779954166. PMID 11453506. S2CID 24763664.
- ^ Naumann A, Rotter N, Bujía J, Aigner J (1998). "Tissue engineering of autologous cartilage transplants for rhinology". American Journal of Rhinology. 12 (1): 59–63. doi:10.2500/105065898782102972. PMID 9513661. S2CID 37632669.
- ^ a b c Malda J, Kreijveld E, Temenoff JS, van Blitterswijk CA, Riesle J (December 2003). "Expansion of human nasal chondrocytes on macroporous microcarriers enhances redifferentiation". Biomaterials. 24 (28): 5153–5161. doi:10.1016/s0142-9612(03)00428-9. PMID 14568432.
- ^ a b c Scotti C, Osmokrovic A, Wolf F, Miot S, Peretti GM, Barbero A, Martin I (February 2012). "Response of human engineered cartilage based on articular or nasal chondrocytes to interleukin-1β and low oxygen". Tissue Engineering. Part A. 18 (3–4): 362–372. doi:10.1089/ten.TEA.2011.0234. PMC 3267974. PMID 21902467.
- ^ a b c Farhadi J, Fulco I, Miot S, Wirz D, Haug M, Dickinson SC, et al. (December 2006). "Precultivation of engineered human nasal cartilage enhances the mechanical properties relevant for use in facial reconstructive surgery". Annals of Surgery. 244 (6): 978–85, discussion 985. doi:10.1097/01.sla.0000247057.16710.be. PMC 1856618. PMID 17122623.
- ^ do Amaral RJ, Pedrosa C, Kochem MC, Silva KR, Aniceto M, Claudio-da-Silva C, et al. (March 2012). "Isolation of human nasoseptal chondrogenic cells: a promise for cartilage engineering". Stem Cell Research. 8 (2): 292–299. doi:10.1016/j.scr.2011.09.006. PMID 22099383.
- ^ Barandun M, Iselin LD, Santini F, Pansini M, Scotti C, Baumhoer D, et al. (August 2015). "Generation and characterization of osteochondral grafts with human nasal chondrocytes". Journal of Orthopaedic Research. 33 (8): 1111–1119. doi:10.1002/jor.22865. PMID 25994595. S2CID 206142529.
- ^ a b Fulco I, Miot S, Haug MD, Barbero A, Wixmerten A, Feliciano S, et al. (July 2014). "Engineered autologous cartilage tissue for nasal reconstruction after tumour resection: an observational first-in-human trial". Lancet. 384 (9940): 337–346. doi:10.1016/S0140-6736(14)60544-4. PMID 24726477. S2CID 12217253.
- ^ a b Pelttari K, Pippenger B, Mumme M, Feliciano S, Scotti C, Mainil-Varlet P, et al. (August 2014). "Adult human neural crest-derived cells for articular cartilage repair". Science Translational Medicine. 6 (251): 251ra119. doi:10.1126/scitranslmed.3009688. PMID 25163479. S2CID 5520982.
- ^ Dell'Accio F, De Bari C, Luyten FP (July 2001). "Molecular markers predictive of the capacity of expanded human articular chondrocytes to form stable cartilage in vivo". Arthritis and Rheumatism. 44 (7): 1608–1619. doi:10.1002/1529-0131(200107)44:7<1608::AID-ART284>3.0.CO;2-T. PMID 11465712.
- ^ Scott MA, Levi B, Askarinam A, Nguyen A, Rackohn T, Ting K, et al. (March 2012). "Brief review of models of ectopic bone formation". Stem Cells and Development. 21 (5): 655–667. doi:10.1089/scd.2011.0517. PMC 3295855. PMID 22085228.
- ^ Bichara DA, Zhao X, Hwang NS, Bodugoz-Senturk H, Yaremchuk MJ, Randolph MA, Muratoglu OK (October 2010). "Porous poly(vinyl alcohol)-alginate gel hybrid construct for neocartilage formation using human nasoseptal cells". The Journal of Surgical Research. 163 (2): 331–336. doi:10.1016/j.jss.2010.03.070. PMID 20538292.
- ^ Dobratz EJ, Kim SW, Voglewede A, Park SS (2009). "Injectable cartilage: using alginate and human chondrocytes". Archives of Facial Plastic Surgery. 11 (1): 40–47. doi:10.1001/archfacial.2008.509. PMID 19153292.
- ^ Kim SW, Dobratz EJ, Ballert JA, Voglewede AT, Park SS (January 2009). "Subcutaneous implants coated with tissue-engineered cartilage". The Laryngoscope. 119 (1): 62–66. doi:10.1002/lary.20025. PMID 19117288. S2CID 22733319.
- ^ Bermueller C, Schwarz S, Elsaesser AF, Sewing J, Baur N, von Bomhard A, et al. (October 2013). "Marine collagen scaffolds for nasal cartilage repair: prevention of nasal septal perforations in a new orthotopic rat model using tissue engineering techniques". Tissue Engineering. Part A. 19 (19–20): 2201–2214. doi:10.1089/ten.TEA.2012.0650. PMC 3762606. PMID 23621795.
- ^ Elsaesser AF, Bermueller C, Schwarz S, Koerber L, Breiter R, Rotter N (June 2014). "In vitro cytotoxicity and in vivo effects of a decellularized xenogeneic collagen scaffold in nasal cartilage repair". Tissue Engineering. Part A. 20 (11–12): 1668–1678. doi:10.1089/ten.TEA.2013.0365. PMID 24372309.
