User:Ehubbard3/sandbox
Name of Disorder
[edit]Title of Page (scientific and common names)
Overview/Definition
[edit]This section should be an abstract of the wikipedia page. It should include a brief summery of what the disease is, the causes, diagnosis, treatment, management, prevalence, demographics, and prognosis of the disease.
Example from Gunther disease :
Gunther disease, also known as congenital erythropoietic porphyria (CEP), uroporphyrinogen III synthase deficiency and UROS deficiency,[1][2] is a congenital form of erythropoietic porphyria. The word porphyria originated from the Greek word porphura. Porphura actually means “purple pigment”, which, in suggestion, the color that the body fluid changes when a person has Gunther’s disease.[3] It is a rare, autosomal recessive[4] metabolic disorder affecting heme, caused by deficiency of the enzyme uroporphyrinogen cosynthetase.[5] It is extremely rare, with a prevalence estimated at 1 in 1,000,000 or less.[6] There have been times that prior to birth of a fetus, Gunther's disease has been shown to lead to anemia. In milder cases patients have not presented any symptoms until they have reached adulthood. In Gunther's disease, porphyrins are accumulated in the teeth and bones and an increased amount are seen in the plasma, bone marrow, feces, red blood cells, and urine.[7][8]
Signs and symptoms
[edit]This section should the signs and symptoms known to be associated with the genetic disease. This could also include other diseases or disorders that can accompany this disorder. This section may contain subcategories for the different manifestations.
Example from Down syndrome:

Those with Down syndrome nearly always have physical and intellectual disabilities.[1] As adults their mental abilities are typically similar to that of an 8 or 9 year old.[2] They also typically have poor immune function[3] and generally reach developmental milestones at a later age.[4] They have an increased risk of a number of other health problems, including: congenital heart disease, leukemia, thyroid disorders, and mental illness, among others.[5]
| Characteristics | Percentage | Characteristics | Percentage |
|---|---|---|---|
| Mental impairment | 99%[6] | Abnormal teeth | 60%[7] |
| Stunted growth | 90%[8] | Slanted eyes | 60%[3] |
| Umbilical hernia | 90%[9] | Shortened hands | 60%[7] |
| Increased skin back of neck | 80%[5] | Short neck | 60%[7] |
| Low muscle tone | 80%[10] | Obstructive sleep apnea | 60%[5] |
| Narrow roof of mouth | 76%[7] | Bent fifth finger tip | 57%[3] |
| Flat head | 75%[3] | Brushfield spots in the iris | 56%[3] |
| Flexible ligaments | 75%[3] | Single transverse palmar crease | 53%[3] |
| Large tongue | 75%[10] | Protruding tongue | 47%[7] |
| Abnormal outer ears | 70%[5] | Congenital heart disease | 40%[7] |
| Flattened nose | 68%[3] | Strabismus | ~35%[11] |
| Separation of 1st and 2nd toes | 68%[7] | Undescended testicles | 20%[12] |
Physical
[edit]
People with Down syndrome may have some or all of the following physical characteristics: a small chin, slanted eyes, poor muscle tone, a flat nasal bridge, a single crease of the palm, and a protruding tongue due to a small mouth and large tongue.[10] These airway changes lead to obstructive sleep apnea in around half of those with Down syndrome.[5] Other common features include: a flat and wide face,[10] a short neck, excessive joint flexibility, extra space between big toe and second toe, abnormal patterns on the fingertips and short fingers.[7][10] Instability of the atlanto-axial joint occurs in approximately 20% and may lead to spinal cord injury in 1–2%.[2][4] Hip dislocations may occur without trauma in up to a third of people with Down syndrome.[5]
Growth in height is slower resulting in adults who tend to have short stature—the average height for men is 154 cm (5 feet 1 inch) and for women is 142 cm (4 feet 8 inches).[13] Individuals with Down syndrome are at increased risk for obesity as they age.[5] There are growth charts specifically for children with Down syndrome.[5]
Neurological
[edit]Most individuals with Down syndrome have mild (IQ: 50–70) or moderate (IQ: 35–50) intellectual disability with some cases having severe (IQ: 20–35) difficulties.[11][14] Those with mosaic Down syndrome typically have IQ scores 10–30 points higher.[15] As they age people with Down syndrome typically perform less well compared to their same-age peers.[14][16] Some after 30 years of age may lose their ability to speak.[2] This syndrome causes about a third of cases of intellectual disability.[3] Many developmental milestones are delayed with the ability to crawl typically occurring around 8 months rather than 5 month and the ability to walk independently typically occurring around 21 months rather than 14 months.[17]
Commonly individuals with Down syndrome have better language understanding than ability to speak.[5][14] Between 10 and 45 percent have either a stutter or rapid and irregular speech, making it difficult to understand them.[18] They typically do fairly well with social skills.[5] Behavior problems are not generally as great an issue as in other syndromes associated with intellectual disability.[14] In children with Down syndrome mental illness occurs in nearly 30% with autism occurring in 5–10%.[4] People with Down syndrome experience a wide range of emotions.[19] While generally happy,[20] symptoms of depression and anxiety may develop in early adulthood.[2]
Children and adults with Down syndrome are at increased risk of epileptic seizures which occur in 5–10% of children and up to 50% of adults.[2] This includes an increased risk of a specific type of seizure called infantile spasms.[5] Many (15%) who live 40 years or longer develop dementia of the Alzheimer's type.[21] In those who reach 60 years of age, 50–70% have the disease.[2]
Senses
[edit]
Hearing and vision disorders occur in more than half of people with Down syndrome.[5] Vision problems occur in 38 to 80%.[11] Between 20 and 50% have strabismus, in which the two eyes do not move together.[11] Cataracts (cloudiness of the len of the eye) occur in 15%,[4] and may be present at birth.[11] Keratoconus (a thin, cone-shaped corneas)[2] and glaucoma (increased eye pressure) are also more common,[11] as are refractive errors requiring glasses or contacts.[2] Brushfield spots (small white or grayish/brown spots on the outer part of the iris) are present in 38 to 85% of individuals.[11]
Hearing problems are found in 50–90% of children with Down syndrome.[22] This is often the result of otitis media with effusion which occurs in 50–70%[4] and chronic ear infections which occurs in 40 to 60%.[23] Ear infections often begin in the first year of life and are partly due to poor eustachian tube function.[24][25] Excessive ear wax can also cause hearing loss due to obstruction of the outer ear canal.[2] Even a mild degree of hearing loss can have negative consequences for speech, language understanding and academics.[11][25] Additionally, it is important to rule out hearing loss as a factor in social and cognitive deterioration.[26] Age-related hearing loss of the sensorineural type occurs at a much earlier age and affects 10–70%.[2]
Heart
[edit]The rate of congenital heart disease in newborns with Down syndrome is around 40%.[7] Of those with heart heart disease about 80% have an atrioventricular septal defect or ventricular septal defect.[2] Mitral valve problems become common as people age, even in those without heart problems at birth.[2] Other problems that may occur include: tetralogy of Fallot and patent ductus arteriosus.[24] People with Down syndrome have a lower risk of hardening of the arteries.[2]
Cancer
[edit]Although the overall risk of cancer is not changed;[27] there is an increased risk of leukemia and testicular cancer and a reduced risk of solid cancers.[2] Solid cancers are believed to be less common due to increased expression of tumor suppressor genes present on chromosome 21.[28]
Cancers of the blood are 10 to 15 times more common in children with Down syndrome.[5] In particular, acute lymphoblastic leukemia is 20 times more common and the megakaryoblastic form of acute myelogenous leukemia is 500 times more common.[29] Transient myeloproliferative disease, a disorder of blood cell production that does not occur outside of Down syndrome, affects 3–10% of infants.[29][30] The disorder is typically not serious but occasionally can be.[30] It resolves most times without treatment; however, in those who have had it there is a 20 to 30 percent risk of developing acute lymphoblastic leukemia at a later time.[30]
Endocrine
[edit]Problems of the thyroid gland occur in 20–50% of individuals with Down syndrome.[2][5] Low thyroid is the most common form, occurring in almost half of all individuals.[2] Thyroid problems can be due to a poorly or non functioning thyroid at birth (known as congenital hypothyroidism) which occurs in 1%[4] or can develop later due to an attack on the thyroid by the immune system resulting in Graves disease or autoimmune hypothyroidism.[31] Type 1 diabetes mellitus is also more common.[2]
Gastrointestinal
[edit]Constipation occurs in nearly half of people with Down syndrome and may result in changes in behavior.[5] One potential cause is Hirschsprung's disease, which is due to a lack of nerve cells controlling the colon, which occurs in 2 to 15%.[32] Other frequent congenital problems include: duodenal atresia, pyloric stenosis, Meckel diverticulum and imperforate anus.[24] Celiac disease affects about 7–20%[2][5] and gastroesophageal reflux disease is also more common.[24]
Fertility
[edit]Males with Down syndrome usually do not father children, while females have lower rates of fertility relative those who are unaffected.[33] Fertility is estimated to be present in 30–50% of women.[34] Menopause typically occurs at an earlier age.[2] The poor fertility in men is thought to be due to problems with sperm development; however, it may also be related to not being sexually active.[33] As of 2006 there have been three recorded instances of males with Down syndrome fathering children and 26 cases of women having children.[33] Without assisted reproductive technologies, approximately half of the pregnancies of someone with Down syndrome will also have the syndrome.[33][35]
Diagnosis
[edit]This section should include what tools and tests are used to diagnose the disease.
Example from Achondroplasia:
Achondroplasia can be detected before birth by the use of prenatal ultrasound. A DNA test can be performed before birth to detect homozygosity, wherein two copies of the mutant gene are inherited, a lethal condition leading to stillbirths. Clinical features include megalocephaly, short limbs, prominent forehead, thoracolumbar kyphosis and mid-facial hypoplasia.[36] Complications like dental malocclusion, hydrocephalus and repeated otitis media can be observed.[36] The risk of death in infancy is increased due to the likelihood of compression of the spinal cord with or without upper airway obstruction.
Radiologic findings
[edit]Achondroplasia is an autosomal dominant anomaly that affects the cartilage growth and development. The individual is a short-limbed dwarf with a relatively normal sized trunk, large head, frontal bossing, and a depressed nasal bridge.
Ultrasound
[edit]- The diagnosis can be made by fetal ultrasound by progressive discordance between the femur length and biparietal diameter by age. The trident hand configuration can be seen if the fingers are fully extended.
- A skeletal survey is useful to confirm the diagnosis of achondroplasia.
Skull
[edit]- The skull is large, with a small, narrow foramen magnum and relatively small skull base.
Limbs
[edit]- Short, wide tubular bones with metaphyseal cupping and flaring and irregular growth plates. Fibular overgrowth is present.
- The hand is broad with short metacarpals and phalanges, and a trident configuration.
- ‘Trident hand’: the fingers are all the same length and diverge into two pairs
- ‘Chevron’ deformity: V-shaped growth plate notches
Thorax
[edit]- Short ribs with cupped anterior ends.
Vertebrae
[edit]- A decreasing interpedicular distance within the lumbar spine (travelling caudally)
- Short vertebral pedicles
- Posterior vertebral body scalloping
- ‘Bullet-shaped’ vertebral bodies: with an anteroinferior anterior beak
- The vertebral bodies are short and flattened with relatively large intervertebral disk height, and there is congenitally narrowed spinal canal.
- Thoracolumbar gibbus in infancy.
Pelvis
[edit]- ‘Tombstone’ appearance: squared small iliac wings with a small sciatic notch
- ‘Champagne glass’ pelvis: the pelvic inlet resembles a champagne glass
- Flat acetabular roofs
- The iliac wings are small and squared,[37] with a narrow sciatic notch and horizontal acetabular roof.
If the radiographic features are not classic, a search for a different diagnosis should be entertained.
Because of the extremely deformed bone structure, people with achondroplasia are often "double jointed".
Another distinct characteristic of the syndrome is thoracolumbar gibbus in infancy.
Treatment and Prognosis
[edit]This section has current accepted treatments for the symptoms of the disease, their availability, and the prognosis of a typical affected individual.
Example from Duchenne muscular dystrophy
There is no current cure for DMD, although phase 1-2a trials with exon-skipping treatment for certain mutations have halted decline and produced small clinical improvements in walking.
Treatment is generally aimed at controlling the onset of symptoms to maximize the quality of life, and include the following:
- Corticosteroids such as prednisolone and deflazacort increase energy and strength and defer severity of some symptoms.[38]
- Randomised control trials have shown that beta2-agonists increase muscle strength but do not modify disease progression. Follow-up time for most RCTs on beta2-agonists is only around 12 months and hence results cannot be extrapolated beyond that time frame. [citation needed]
- Mild, non-jarring physical activity such as swimming is encouraged. Inactivity (such as bed rest) can worsen the muscle disease.
- Physical therapy is helpful to maintain muscle strength, flexibility, and function.
- Orthopedic appliances (such as braces and wheelchairs) may improve mobility and the ability for self-care. Form-fitting removable leg braces that hold the ankle in place during sleep can defer the onset of contractures.
- Appropriate respiratory support as the disease progresses is important.
Comprehensive multi-disciplinary care standards/guidelines for DMD have been developed by the Centers for Disease Control and Prevention (CDC), and were published in two parts in The Lancet Neurology in 2010. To download the two articles in PDF format, go to the TREAT-NMD website.[39]
Prognosis
[edit]Duchenne muscular dystrophy is a progressive disease which eventually affects all voluntary muscles and involves the heart and breathing muscles in later stages. The life expectancy is currently estimated to be around 25,[40] but this varies from patient to patient. Recent advancements in medicine are extending the lives of those afflicted. The Muscular Dystrophy Campaign, which is a leading UK charity focusing on all muscle disease, states that "with high standards of medical care young men with Duchenne muscular dystrophy are often living well into their 30s".[41]
In rare cases, persons with DMD have been seen to survive into the forties or early fifties, with the use of proper positioning in wheelchairs and beds, ventilator support (via tracheostomy or mouthpiece), airway clearance, and heart medications, if required.[citation needed] Early planning of the required supports for later-life care has shown greater longevity in people living with DMD.
Physical therapy
[edit]Physical therapists are concerned with enabling children to reach their maximum physical potential. Their aim is to:
- minimize the development of contractures and deformity by developing a programme of stretches and exercises where appropriate
- anticipate and minimize other secondary complications of a physical nature
- monitor respiratory function and advise on techniques to assist with breathing exercises and methods of clearing secretions
Mechanical ventilatory/respiration assistance
[edit]Modern "volume ventilators/respirators," which deliver an adjustable volume (amount) of air to the person with each breath, are valuable in the treatment of people with muscular dystrophy related respiratory problems. The ventilator may require an invasive endotracheal or tracheotomy tube through which air is directly delivered, but, for some people non-invasive delivery through a face mask or mouthpiece is sufficient. Positive airway pressure machines, particularly bi-level ones, are sometimes used in this latter way. The respiratory equipment may easily fit on a ventilator tray on the bottom or back of a power wheelchair with an external battery for portability.
Ventilator treatment may start in the mid to late teens when the respiratory muscles can begin to collapse. If the vital capacity has dropped below 40 percent of normal, a volume ventilator/respirator may be used during sleeping hours, a time when the person is most likely to be under ventilating ("hypoventilating"). Hypoventilation during sleep is determined by a thorough history of sleep disorder with an oximetry study and a capillary blood gas (See Pulmonary Function Testing).
If the vital capacity continues to decline to less than 30 percent of normal, a volume ventilator/respirator may also be needed during the day for more assistance. The person gradually will increase the amount of time using the ventilator/respirator during the day as needed.
However, there are also people with the disease in their 20's who have no need for a ventilator.
Genetic Basis
[edit]The genetic components of the disease. Specific genes, proteins, or molecular pathways can be described based on what is known. The mechanisms by which the genetic mutations occur, or whether the disease results from a pattern of mutations(such as in retinoblastoma) are in this section.
Example from Huntington's disease:
All humans have two copies of the Huntingtin gene (HTT), which codes for the protein Huntingtin (Htt). The gene is also called HD and IT15, which stands for 'interesting transcript 15'. Part of this gene is a repeated section called a trinucleotide repeat, which varies in length between individuals and may change length between generations. If the repeat is present in a healthy gene, a dynamic mutation may increase the repeat count and result in a defective gene. When the length of this repeated section reaches a certain threshold, it produces an altered form of the protein, called mutant Huntingtin protein (mHtt). The differing functions of these proteins are the cause of pathological changes which in turn cause the disease symptoms. The Huntington's disease mutation is genetically dominant and almost fully penetrant: mutation of either of a person's HTT genes causes the disease. It is not inherited according to sex, but the length of the repeated section of the gene and hence its severity can be influenced by the sex of the affected parent.[42]
Genetic mutation
[edit]HD is one of several trinucleotide repeat disorders which are caused by the length of a repeated section of a gene exceeding a normal range.[43] The HTT gene is located on the short arm of chromosome 4[43] at 4p16.3. HTT contains a sequence of three DNA bases—cytosine-adenine-guanine (CAG)—repeated multiple times (i.e. ... CAGCAGCAG ...), known as a trinucleotide repeat.[43] CAG is the 3-letter genetic code (codon) for the amino acid glutamine, so a series of them results in the production of a chain of glutamine known as a polyglutamine tract (or polyQ tract), and the repeated part of the gene, the PolyQ region.[44]
| Repeat count | Classification | Disease status | Risk to offspring |
|---|---|---|---|
| <26 | Normal | Will not be affected | None |
| 27–35 | Intermediate | Will not be affected | Elevated but <<50% |
| 36–39 | Reduced Penetrance | May or may not be affected | 50% |
| 40+ | Full Penetrance | Will be affected | 50% |
Generally, people have fewer than 36 repeated glutamines in the polyQ region which results in production of the cytoplasmic protein Huntingtin.[43] However, a sequence of 36 or more glutamines results in the production of a protein which has different characteristics.[43] This altered form, called mHtt (mutant Htt), increases the decay rate of certain types of neurons. Regions of the brain have differing amounts and reliance on these type of neurons, and are affected accordingly.[45] Generally, the number of CAG repeats is related to how much this process is affected, and accounts for about 60% of the variation of the age of the onset of symptoms. The remaining variation is attributed to environment and other genes that modify the mechanism of HD.[43] 36–39 repeats result in a reduced-penetrance form of the disease, with a much later onset and slower progression of symptoms. In some cases the onset may be so late that symptoms are never noticed.[46] With very large repeat counts, HD has full penetrance and can occur under the age of 20, when it is then referred to as juvenile HD, akinetic-rigid, or Westphal variant HD. This accounts for about 7% of HD carriers.[47]
Inheritance
[edit]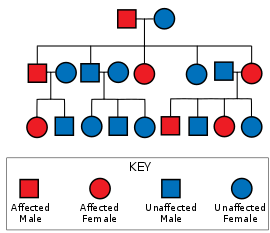
Huntington's disease has autosomal dominant inheritance, meaning that an affected individual typically inherits one copy of the gene with an expanded trinucleotide repeat (the mutant allele) from an affected parent.[48] Since penetrance of the mutation is very high, those who have a mutated copy of the gene will have the disease. In this type of inheritance pattern, each offspring of an affected individual has a 50% risk of inheriting the mutant allele and therefore being affected with the disorder (see figure). This probability is sex-independent.[49]
Trinucleotide CAG repeats over 28 are unstable during replication and this instability increases with the number of repeats present.[46] This usually leads to new expansions as generations pass (dynamic mutations) instead of reproducing an exact copy of the trinucleotide repeat.[43] This causes the number of repeats to change in successive generations, such that an unaffected parent with an "intermediate" number of repeats (28–35), or "reduced penetrance" (36–40), may pass on a copy of the gene with an increase in the number of repeats that produces fully penetrant HD.[43] Such increases in the number of repeats (and hence earlier age of onset and severity of disease) in successive generations is known as genetic anticipation.[43] Instability is greater in spermatogenesis than oogenesis;[43] maternally inherited alleles are usually of a similar repeat length, whereas paternally inherited ones have a higher chance of increasing in length.[43][50] It is rare for Huntington's disease to be caused by a new mutation, where neither parent has over 36 CAG repeats.[51]
In the rare situations where both parents have an expanded HD gene, the risk increases to 75%, and when either parent has two expanded copies, the risk is 100% (all children will be affected). Individuals with both genes affected are rare. For some time HD was thought to be the only disease for which possession of a second mutated gene did not affect symptoms and progression,[52] but it has since been found that it can affect the phenotype and the rate of progression.[43][53]
Epidemiology
[edit]This section should include the incidence, distribution, and possible control of the genetic disease.
Example from Sickle-cell disease:
The highest frequency of sickle cell disease is found in tropical regions, particularly sub-Saharan Africa, India and the Middle-East.[54] Migration of substantial populations from these high prevalence areas to low prevalence countries in Europe has dramatically increased in recent decades and in some European countries sickle cell disease has now overtaken more familiar genetic conditions such as haemophilia and cystic fibrosis.[55] In 2010, there were about 29,000 deaths attributed to sickle cell disease globally.[56]
Africa
[edit]Three quarters of sickle-cell cases occur in Africa. A recent WHO report estimated that around 2% of newborns in Nigeria were affected by sickle cell anaemia, giving a total of 150,000 affected children born every year in Nigeria alone. The carrier frequency ranges between 10% and 40% across equatorial Africa, decreasing to 1–2% on the north African coast and <1% in South Africa.[57]
United States
[edit]The prevalence of the disease in the United States is approximately 1 in 5,000, mostly affecting Americans of Sub-Saharan African descent, according to the National Institutes of Health.[58] In the United States, about 1 out of 500 African-American children and 1 in every 36,000 Hispanic-American children born will have sickle-cell anaemia.[59] It is estimated that Sickle Cell Disease (SCD) affects 90,000 Americans.[60] Most infants with SCD born in the United States are now identified by routine neonatal screening. Forty-four states along with the District of Columbia, Puerto Rico and the Virgin Islands currently provide universal neonatal screening for SCD.[61][62] Sickle Cell trait occurs among about 1:12 African-Americans and 1:100 Hispanic-Americans.[63] It is estimated that 2.5 million Americans are heterozygous carriers for the sickle cell trait.[64]
France
[edit]As a result of population growth in African-Caribbean regions of overseas France and immigration from North and sub-Saharan Africa to mainland France, sickle cell disease has become a major health problem in France.[65] SCD has become the most common genetic disease in the country, with an overall birth prevalence of 1/2,415 in mainland France, ahead of phenylketonuria (1/10,862), congenital hypothyroidism (1/3,132), congenital adrenal hyperplasia (1/19,008) and cystic fibrosis (1/5,014) for the same reference period. In 2010, 31.5% of all newborns in mainland France (253,466 out of 805,958) were screened for SCD (this percentage was 19% in 2000). 341 newborns with SCD and 8,744 heterozygous carriers were found representing 1.1% of all newborns in mainland France. The Paris metropolitan district (Île-de-France) is the region that accounts for the largest number of newborns screened for SCD (60% in 2010). The second largest number of at-risk is in Provence-Alpes-Côte d'Azur at nearly 43.2% and the lowest number is in Brittany at 5.5%.[66][67]
United Kingdom
[edit]In the United Kingdom, all babies receive a blood test to screen for this condition.[68]
Middle East
[edit]In Saudi Arabia about 4.2% of the population carry the sickle-cell trait and 0.26% have sickle cell disease. The highest prevalence is in the Eastern province where approximately 17% of the population carry the gene and 1.2% have sickle cell disease.[69] In 2005 in Saudi Arabia a mandatory pre-marital test including HB electrophoresis was launched and aimed to decrease the incidence of SCD and thalassemia.[70]
India
[edit]Sickle cell disease is common in many parts of India, where the prevalence has ranged from 9.4 to 22.2% in endemic areas.[71]
Caribbean Islands
[edit]In Jamaica, 10% of the population carries the sickle cell gene, making it the most prevalent genetic disorder in the country.[72]
History
[edit]This section explains historical significance. It will include the original identification of the disease or syndrome and how it was named. Noteworthy case studies, or related advancements in diagnosis and treatment methods can also be included.
Example from Haemophilia
"About seventy or eighty years ago, a woman by name of Smith, settled in the vicinity of Plymouth, New Hampshire, and transmitted the following idiosyncrasy to her descendants. It is one, she observed, to which her family is unfortunately subject, and had been the source not only of great solicitude, but frequently the cause of death. If the least scratch is made on the skin of some of them, as mortal a hemorrhagy will eventually ensue as if the largest wound is inflicted. (…) So assured are the members of this family of the terrible consequences of the least wound, that they will not suffer themselves to be bled on any consideration, having lost a relation by not being able to stop the discharge occasioned by this operation."
John C. Otto, 1803[73]
Scientific discovery
[edit]The first medical professional to describe a disease was Abulcasis. In the tenth century he described families whose males died of bleeding after only minor traumas.[74] While many other such descriptive and practical references to the disease appear throughout historical writings, scientific analysis did not begin until the start of the nineteenth century.
In 1803, Dr. John Conrad Otto, a Philadelphian physician, wrote an account about "a hemorrhagic disposition existing in certain families" in which he called the affected males "bleeders".[75] He recognised that the disorder was hereditary and that it affected mostly males and was passed down by healthy females. His paper was the second paper to describe important characteristics of an X-linked genetic disorder (the first paper being a description of colour blindness by John Dalton who studied his own family). Otto was able to trace the disease back to a woman who settled near Plymouth in 1720. The idea that affected males could pass the trait onto their unaffected daughters was not described until 1813 when John Hay published an account in The New England Journal of Medicine.[76][77]
In 1924, a Finnish doctor discovered a hereditary bleeding disorder similar to Haemophilia localised in a group of islands (called the "Åland Islands") which are located to the southwest of Finland.[78] This bleeding disorder is called "Von Willebrand Disease".
The term "haemophilia" is derived from the term "haemorrhaphilia" which was used in a description of the condition written by Friedrich Hopff in 1828, while he was a student at the University of Zurich.[75][79] In 1937, Patek and Taylor, two doctors from Harvard, discovered anti-haemophilic globulin.[80] In 1947, Pavlosky, a doctor from Buenos Aires, found haemophilia A and haemophilia B to be separate diseases by doing a lab test. This test was done by transferring the blood of one haemophiliac to another haemophiliac. The fact that this corrected the clotting problem showed that there was more than one form of haemophilia.
European royalty
[edit]
Haemophilia has featured prominently in European royalty and thus is sometimes known as 'the royal disease'. Queen Victoria passed the mutation for Haemophilia B[81][82] to her son Leopold and, through some of her daughters, to various royals across the continent, including the royal families of Spain, Germany, and Russia. In Russia, Tsarevich Alexei Nikolaevich, son of Nicholas II, was a descendant of Queen Victoria through his mother Empress Alexandra and suffered from haemophilia.
It was claimed that Rasputin was successful at treating Tsarevich's haemophilia. At the time, a common treatment administered by professional doctors was to use aspirin, which worsened rather than lessened the problem. It is believed that, by simply advising against the medical treatment, Rasputin could bring visible and significant improvement to the condition of Tsarevich.
In Spain, Queen Victoria's youngest daughter, Princess Beatrice, had a daughter Victoria Eugenie of Battenberg, who later became Queen of Spain. Two of her sons were haemophiliacs and both died from minor car accidents. Her eldest son, Prince Alfonso of Spain, Prince of Asturias, died at the age of 31 from internal bleeding after his car hit a telephone booth. Her youngest son, Infante Gonzalo, died at age 19 from abdominal bleeding following a minor car accident where he and his sister hit a wall while avoiding a cyclist. Neither appeared injured or sought immediate medical care and Gonzalo died two days later from internal bleeding.
Blood contamination issues
[edit]
Prior to 1985, there were no laws enacted within the U.S. to screen blood. As a result, many haemophilia patients who received untested and unscreened clotting factor prior to 1992 were at an extreme risk for contracting HIV and hepatitis C via these blood products. It is estimated that more than 50% of the haemophilia population, i.e. over 10,000 people, contracted HIV from the tainted blood supply in the United States alone.[83]
As a direct result of the contamination of the blood supply in the late 1970s and early/mid-1980s with viruses such as hepatitis and HIV, new methods were developed in the production of clotting factor products. The initial response was to heat-treat (pasteurise) plasma-derived factor concentrate, followed by the development of monoclonal factor concentrates, which use a combination of heat treatment and affinity chromatography to inactivate any viral agents in the pooled plasma from which the factor concentrate is derived. The Lindsay Tribunal in Ireland investigated, among other things, the slow adoption of the new methods.
References
[edit]See Also
[edit]External links
[edit]Table
[edit]This template's initial visibility currently defaults to autocollapse, meaning that if there is another collapsible item on the page (a navbox, sidebar, or table with the collapsible attribute), it is hidden apart from its title bar; if not, it is fully visible.
To change this template's initial visibility, the |state= parameter may be used:
{{Ehubbard3|state=collapsed}}will show the template collapsed, i.e. hidden apart from its title bar.{{Ehubbard3|state=expanded}}will show the template expanded, i.e. fully visible.
Category:Heme metabolism disorders Category:Metabolic disorder templates
- ^ Faragher, edited by Rhonda (2013). Educating Learners with Down Syndrome Research, theory, and practice with children and adolescents. Hoboken: Taylor and Francis. p. 5. ISBN 978-1-134-67335-3.
{{cite book}}:|first=has generic name (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c d e f g h i j k l m n o p q r s Cite error: The named reference
Malt2013was invoked but never defined (see the help page). - ^ a b c d e f g h i Cite error: The named reference
Steph2010was invoked but never defined (see the help page). - ^ a b c d e f Cite error: The named reference
Nelson2011was invoked but never defined (see the help page). - ^ a b c d e f g h i j k l m n o p Hickey, Fran; Hickey, Erin; Summar, Karen L. (2012). "Medical update for children with Down syndrome for the pediatrician and family practitioner". Advances in Pediatrics. 59 (1): 137–57. doi:10.1016/j.yapd.2012.04.006. PMID 22789577.
{{cite journal}}: CS1 maint: date and year (link) - ^ Sankar, editors John M. Pellock, Blaise F.D. Bourgeois, W. Edwin Dodson ; associate editors, Douglas R. Nordli, Jr., Raman (2008). Pediatric epilepsy diagnosis and therapy (3rd ed.). New York: Demos Medical Pub. p. Chapter 67. ISBN 978-1-934559-86-4.
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ a b c d e f g h i Epstein, Charles J. (2007). The consequences of chromosome imbalance : principles, mechanisms, and models. Cambridge: Cambridge University Press. pp. 255–256. ISBN 978-0-521-03809-6.
- ^ Daniel Bernstein (2012). Pediatrics for medical students (3rd ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 259. ISBN 978-0-7817-7030-9.
- ^ Tecklin, Jan S. (2008). Pediatric physical therapy (4th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 380. ISBN 978-0-7817-5399-9.
- ^ a b c d e Domino, edited by Frank J. (2007). The 5-minute clinical consult 2007 (2007 ed.). Philadelphia: Lippincott Williams & Wilkins. p. 392. ISBN 978-0-7817-6334-9.
{{cite book}}:|first=has generic name (help) - ^ a b c d e f g h Cite error: The named reference
Wei2010was invoked but never defined (see the help page). - ^ Wilson, Golder N. (2006). Preventive management of children with congenital anomalies and syndromes (2 ed.). Cambridge: Cambridge University Press. p. 190. ISBN 978-0-521-61734-5.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Williams Textbook of Endocrinology Expert Consult (12th ed.). London: Elsevier Health Sciences. 2011. ISBN 978-1-4377-3600-7.
- ^ a b c d Reilly, C (Oct 2012). "Behavioural phenotypes and special educational needs: is aetiology important in the classroom?". Journal of Intellectual Disability Research : JIDR. 56 (10): 929–46. doi:10.1111/j.1365-2788.2012.01542.x. PMID 22471356.
- ^ Batshaw, Mark, ed. (2005). Children with disabilities (5th ed.). Baltimore [u.a.]: Paul H. Brookes. p. 308. ISBN 978-1-55766-581-2.
- ^ Patterson, T.; Rapsey, C. M.; Glue, P. (Apr 2013). "Systematic review of cognitive development across childhood in Down syndrome: implications for treatment interventions". Journal of Intellectual Disability Research : JIDR. 57 (4): 306–18. doi:10.1111/jir.12037. PMID 23506141.
- ^ Rondal, edited by Jean-Adolphe (2007). Therapies and rehabilitation in Down syndrome. Chichester, England: J. Wiley & Sons. p. 116. ISBN 978-0-470-31997-0.
{{cite book}}:|first=has generic name (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Kent, R. D.; Vorperian, H. K. (Feb 2013). "Speech impairment in Down syndrome: a review". Journal of Speech, Language, and Hearing Research : JSLHR. 56 (1): 178–210. doi:10.1044/1092-4388(2012/12-0148). PMC 3584188. PMID 23275397.
- ^ McGuire, Dennis and Chicoine, Brian (2006). Mental Wellness in Adults with Down Syndrome. Bethesday, MD: Woodbine House, Inc. p. 49. ISBN 1-890627-65-8.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Margulies, Phillip (2007). Down syndrome (1st ed.). New York: Rosen Pub. Group. p. 5. ISBN 978-1-4042-0695-3.
- ^ M. William Schwartz, ed. (2012). The 5-minute pediatric consult (6th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 289. ISBN 978-1-4511-1656-4.
- ^ Cite error: The named reference
Rod2012was invoked but never defined (see the help page). - ^ Evans-Martin, F. Fay (2009). Down syndrome. New York: Chelsea House. p. 71. ISBN 978-1-4381-1950-2.
- ^ a b c d Tintinalli, Judith E. (2010). "The Child with Special Health Care Needs". Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). New York: McGraw-Hill Companies. pp. Chapter 138. ISBN 978-0-07-148480-0.
- ^ a b Sam Goldstein, ed. (2011). Handbook of neurodevelopmental and genetic disorders in children (2nd ed.). New York: Guilford Press. p. 365. ISBN 978-1-60623-990-2.
- ^ editor, Vee P. Prasher (2009). Neuropsychological assessments of dementia in Down syndrome and intellectual disabilities. London: Springer. p. 56. ISBN 978-1-84800-249-4.
{{cite book}}:|last=has generic name (help) - ^ Richard Urbano (9 September 2010). Health Issues Among Persons With Down Syndrome. Academic Press. p. 129. ISBN 978-0-12-374477-7.
- ^ Andrei Thomas-Tikhonenko, ed. (2010). Cancer genome and tumor microenvironment (Online-Ausg. ed.). New York: Springer. p. 203. ISBN 978-1-4419-0711-0.
- ^ a b Seewald, Laura; Taub, Jeffrey W.; Maloney, Kelly W.; McCabe, Edward R.B. (Sep 2012). "Acute leukemias in children with Down syndrome". Molecular Genetics and Metabolism. 107 (1–2): 25–30. doi:10.1016/j.ymgme.2012.07.011. PMID 22867885.
- ^ a b c Gamis, A. S.; Smith, F. O. (Nov 2012). "Transient myeloproliferative disorder in children with Down syndrome: clarity to this enigmatic disorder". British Journal of Haematology. 159 (3): 277–87. doi:10.1111/bjh.12041. PMID 22966823.
- ^ Graber, Evan; Chacko, Elizabeth; Regelmann, Molly O.; Costin, Gertrude; Rapaport, Robert (Dec 2012). "Down syndrome and thyroid function". Endocrinology and Metabolism Clinics of North America. 41 (4): 735–45. doi:10.1016/j.ecl.2012.08.008. PMID 23099267.
- ^ Moore, SW (Aug 2008). "Down syndrome and the enteric nervous system". Pediatric Surgery International. 24 (8): 873–83. doi:10.1007/s00383-008-2188-7. PMID 18633623.
- ^ a b c d Pradhan, M; Dalal, A; Khan, F; Agrawal, S (2006). "Fertility in men with Down syndrome: a case report". Fertil Steril. 86 (6): 1765.e1–3. doi:10.1016/j.fertnstert.2006.03.071. PMID 17094988.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cite error: The named reference
Nel2010was invoked but never defined (see the help page). - ^ Cite error: The named reference
Rubin2013was invoked but never defined (see the help page). - ^ a b Beattie, R.M.; Champion, M.P., ed. (2004). Essential questions in paediatrics for MRCPCH (1st ed.). Knutsford, Cheshire: PasTest. ISBN 1-901198-99-5.
{{cite book}}: CS1 maint: multiple names: editors list (link) - ^ "Achondroplasia Pelvis". Archived from the original on 2007-10-22. Retrieved 2007-11-28.
- ^ Mendell, J. R.; Moxley, R. T.; Griggs, R. C.; Brooke, M. H.; Fenichel, G. M.; Miller, J. P.; King, W.; Signore, L.; Pandya, S.; Florence, J.; Schierbecker, J.; Robison, J.; Kaiser, K.; Mandel, S.; Arfken, C.; Gilder, B. (1989). "Randomized, Double-Blind Six-Month Trial of Prednisone in Duchenne's Muscular Dystrophy". New England Journal of Medicine. 320 (24): 1592–1597. doi:10.1056/NEJM198906153202405. PMID 2657428.
- ^ http://www.treat-nmd.eu/downloads/file/standardsofcare/dmd/lancet/the_diagnosis_and_management_of_dmd_lancet_complete_with_erratum.pdf
- ^ Cite error: The named reference
nlmwas invoked but never defined (see the help page). - ^ "Duchenne muscular dystrophy (DMD) | Muscular Dystrophy Campaign". Muscular-dystrophy.org. Retrieved 2013-02-16.
- ^ Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [221]. doi:10.1016/S0140-6736(07)60111-1. PMID 17240289.
- ^ a b c d e f g h i j k l m Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [220]. doi:10.1016/S0140-6736(07)60111-1. PMID 17240289.
- ^ Katsuno M; Banno H; Suzuki K; et al. (2008). "Molecular genetics and biomarkers of polyglutamine diseases". Curr. Mol. Med. 8 (3): 221–34. doi:10.2174/156652408784221298. PMID 18473821. Retrieved 1 April 2009.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Cite error: The named reference
lancet219was invoked but never defined (see the help page). - ^ a b Walker FO (2007). "Huntington's disease". Lancet. 369 (9557): 218–28 [222]. doi:10.1016/S0140-6736(07)60111-1. PMID 17240289.
- ^ Nance MA, Myers RH (2001). "Juvenile onset Huntington's disease—clinical and research perspectives". Ment Retard Dev Disabil Res Rev. 7 (3): 153–7. doi:10.1002/mrdd.1022. PMID 11553930.
- ^ Cite error: The named reference
lancet218was invoked but never defined (see the help page). - ^ Passarge, E (2001). Color Atlas of Genetics (2nd ed.). Thieme. p. 142. ISBN 0-86577-958-9.
- ^ Ridley RM, Frith CD, Crow TJ, Conneally PM (1988). "Anticipation in Huntington's disease is inherited through the male line but may originate in the female". Journal of Medical Genetics. 25 (9): 589–595. doi:10.1136/jmg.25.9.589. PMC 1051535. PMID 2972838.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Semaka A, Creighton S, Warby S, Hayden MR (2006). "Predictive testing for Huntington disease: interpretation and significance of intermediate alleles". Clin. Genet. 70 (4): 283–94. doi:10.1111/j.1399-0004.2006.00668.x. PMID 16965319.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wexler NS; Young AB; Tanzi RE; et al. (1987). "Homozygotes for Huntington's disease". Nature. 326 (6109): 194–197. doi:10.1038/326194a0. PMID 2881213.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Squitieri F; Gellera C; Cannella M; et al. (2003). "Homozygosity for CAG mutation in Huntington disease is associated with a more severe clinical course". Brain. 126 (Pt 4): 946–55. doi:10.1093/brain/awg077. PMID 12615650.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Weatherall DJ, Clegg JB (2001). "Inherited haemoglobin disorders: an increasing global health problem". Bull. World Health Organ. 79 (8): 704–12. PMC 2566499. PMID 11545326.
- ^ Roberts I, de Montalembert M (July 2007). "Sickle cell disease as a paradigm of immigration hematology: new challenges for hematologists in Europe". Haematologica. 92 (7): 865–71. doi:10.3324/haematol.11474. PMID 17606434.
- ^ Lozano, R (Dec 15, 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604.
- ^ WHO. "Sickle-cell anaemia - Report by the Secretariat" (PDF). Retrieved 2010-11-27.
- ^ National Heart, Lung and Blood Institute. "Sickle cell anemia, key points". Retrieved 2010-11-27.
- ^ "September is Sickle Cell Awareness Month". CDC. Retrieved 6 February 2011.
- ^ "Sickle Cell Disease: Data & Statistics". Centers for Disease Control and Prevention. 16 September 2011. Retrieved 8 November 2011.
- ^ American Academy of Pediatrics Section on Hematology/Oncology Committee on Genetics (2002). "Health Supervision for Children with Sickle Cell Disease". Pediatrics. 109 (3): 526–535. doi:10.1542/peds.109.3.526. PMID 11875155.
- ^ Pass KA, Lane PA, Fernhoff PM (2000). "US newborn screening system guidelines II: follow-up of children, diagnosis, management, and evaluation". J Pediatr. 137 (37): S1–S46. doi:10.1067/mpd.2000.109437. PMID 11044838.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Sickle Cell Disease". March of Dimes®. February 2008. Retrieved 8 November 2011.
- ^ Cinnchinsky EP, Mahoney DH, Landlaw SA (29 November 2011). "Uptodate: Sickle Cell Trait". Retrieved 8 November 2011.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Bardakdjian J, Wajcman H (September 2004). "[Epidemiology of sickle cell anemia]". Rev Prat (in French). 54 (14): 1531–3. PMID 15558961.
- ^ Bardakdjian-Michau J, Bahuau M, Hurtrel D; et al. (January 2009). "Neonatal screening for sickle cell disease in France". J. Clin. Pathol. 62 (1): 31–3. doi:10.1136/jcp.2008.058867. PMID 19103855.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Le dépistage néonatal de la drépanocytose en France. Numéro thématique. La drépanocytose en France : des données épidémiologiques pour améliorer la prise en charge, Bardakdjian-Michau J, INVS, July 2012
- ^ http://www.nhs.uk/conditions/sickle-cell-anaemia/Pages/Introduction.aspx
- ^ Jastaniah W (2011). "Epidemiology of sickle cell disease in Saudi Arabia". Annals of Saudi Medicine. 31 (3): 289–93. doi:10.4103/0256-4947.81540. PMC 3119971. PMID 21623060.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Memish ZA, Saeedi MY (2011). "Six-year outcome of the national premarital screening and genetic counseling program for sickle cell disease and β-thalassemia in Saudi Arabia". Annals of Saudi Medicine. 31 (3): 229–35. doi:10.4103/0256-4947.81527. PMC 3119961. PMID 21623050.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Awasthy N, Aggarwal KC, Goyal PC, Prasad MS, Saluja S, Sharma M (2008). "Sickle cell disease: Experience of a tertiary care center in a nonendemic area". Annals of Tropical Medicine and Public Health. 1 (1): 1–4. doi:10.4103/1755-6783.43069.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Asnani, M. R.; McCaw-Binns, A. M.; Reid, M. E. (2011). "Excess Risk of Maternal Death from Sickle Cell Disease in Jamaica: 1998–2007". PLOS ONE. 6 (10): e26281. doi:10.1371/journal.pone.0026281. PMC 3200316. PMID 22039456.
- ^ "Otto JC. The Medical Repository. 1803; Vol VI (1): 1-4". Genmedhist.info. Retrieved 2013-11-21.
- ^ "Case of the Week 175". University of Utah Medical Library. Archived from the original on 19 May 2011.
- ^ a b Nilsson, I. M. (1994). "Haemophilia--then and now". Sydsvenska Medicinhistoriska Sallskapets Arsskrift. 31: 33–52. PMID 11640407.
- ^ DIGITISED EARLY PAPERS AND BOOKS ON HUMAN AND MEDICAL GENETICS Genetics and Medicine Historical Network, Cardiff University.
- ^ Hay J (July 1813). "Account of a remarkable hæmorrhagic disposition, existing in many individuals of the same family". N Engl J Med Surg. 2 (3): 221–5. doi:10.1056/NEJM181307010020302.
- ^ "Haemophilia Special Issue: von Willebrand's Disease: a Report from a Meeting in the Åland Islands". Haemophilia. 18. 2012. doi:10.1111/hae.2012.18.issue-s6. Retrieved 22 November 2012.
- ^ "The History of hemophilia". Retrieved 5 June 2009.
- ^ Chapter 38 Coagulation Factors V and VIII by GC White and GE Gilbert in "Blood: principles and practice of hematology: 2nd edition" 2003. Eds. Robert I. Handin, Samuel E. Lux, Thomas P. Stossel. ISBN 978-0-7817-1993-3
- ^ Michael Price (8 October 2009). "Case Closed: Famous Royals Suffered From Hemophilia". ScienceNOW Daily News. AAAS. Retrieved 9 October 2009.
- ^ Evgeny I. Rogaev; et al. (8 October 2009). "Genotype Analysis Identifies the Cause of the "Royal Disease"". Science. Retrieved 9 October 2009.
{{cite web}}: Explicit use of et al. in:|author=(help) - ^ In re Rhone-Poulenc Rorer Inc., 51 F.3d 1293, 1296 (7th Cir. 1995), Projectposner.org, Retrieved 28 January 2008

